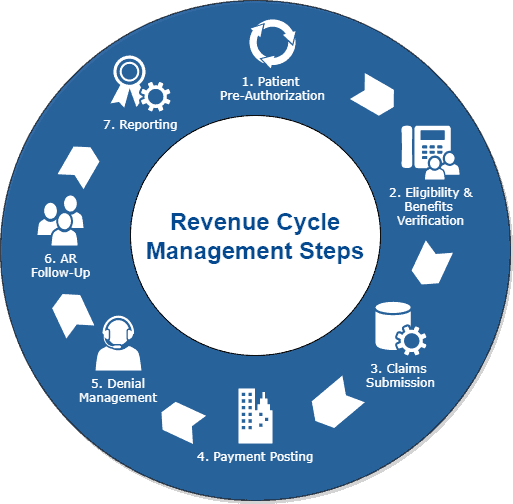
Running a healthcare company successfully depends much on revenue cycle management or RCM. The way a medical company handles its finances and patients determines how seamlessly it functions. From the moment a client schedules an appointment to the time their payment clears, every phase of this process is vital. The degree of money generated, running expenses, and even the quality of treatment received can all be considerably influenced by how well RCM performs.
You must have accuracy and a strategy if you are to negotiate the complex realm of healthcare revenue cycle management. Medical bills evolve with the times as rules and technology develop. Providers must grasp every stage if they want to get the finest financial results for their operations. This blog post will walk you through fifteen key RCM processes and show how to increase performance while ensuring patients receive the best treatment available. Tightly hold on since we are going to delve far into the realm of medical bills cycles!
Step 1: Patient Registration and Scheduling
Getting patients registered and booked marks the first stage in healthcare revenue cycle management. The tone of the entire medical billing process is set in this first phase.
When they register, patients have to provide vital information including their name, phone number, insurance coverage, and medical background. Here, accuracy is quite crucial. Any errors could make the process take more than expected.
Setting appointments fast enables the clinic to maximize its resources. It reduces waiting periods and guarantees that individuals may access providers when they need them. Patients are happier and operations flow more naturally when a seamless scheduling approach is followed.
Talking to patients during this section helps them to develop trust and clarifies for them what to expect from their appointment. The patient’s general feeling is much changed by starting a good relationship.
Correct handling of this first stage prepares you for the following actions including claim filing and insurance verification.
Step 2: Insurance Verification
Managing the healthcare income cycle depends much on confirming insurance. It is the first item examined before any services are offered.
Staff members now verify patient eligibility and review their insurance records. They should learn more about the specifics of their coverage and the advantages relevant for the forthcoming treatment.
Ensuring their insurance is current helps patients prevent surprising expenses. It also reduces later denials of claims, therefore accelerating the RCM process in medical billing.
Proof works best when one is detail-oriented. Making sure that information entered into systems is accurate and compliant with policy falls on staff workers.
Making mistakes at this stage could cause later-on hold-ups or malfunctions. By enabling patients to immediately grasp expenses, a strong procedure here not only saves time but also makes them happier.
Clear talks with insurance providers should be the main focus to ensure that before beginning treatment all areas of coverage are completely known.
Step 3: Coding and Documentation
Managing the healthcare income cycle depends much on paperwork and coding. Correct coding guarantees that the services are converted into the correct invoicing numbers. You have to do this before you can get reimbursed.
Starting the process with specific codes based on clinical data, medical coders enter diagnoses, treatments, and procedures. These figures are created using standards including ICD-10 or CPT. By being exact here, one lowers the possibility of errors that can cause claim denials.
These rules are supported by a lot of evidence proving correct patient care. It must cover any aspect of the visit, from the displayed signs to the administered therapies. Good documentation not only simplifies billing but also helps you to be safe should audits or conflicts arise.
Good recordkeeping and correct reporting are quite important for a medical billing cycle to go without. Simply said, while still adhering to the policies, make sure that service providers are paid accurately and on time for their valuable work.
Step 4: Claims Submission
Managing the healthcare money flow mostly depends on the claims submission. It is the platform where all the thus far accumulated effort comes together.
This is regarding accuracy. Every claim should be filled out with the correct patient information and codes, so care is needed. One error could lead to rejections or delays, therefore affecting cash flow greatly.
Also quite crucial is being on time. Quickly sent claims will enable insurance firms to pay faster, therefore maintaining the flow of money. Usually handling this stage, automated methods expedite the filing procedure.
Keeping an eye on the rules is also vital since they evolve constantly. Keeping current helps you to prevent potential compliance issues.
Effective claims submission shapes the tone of medical billing procedures and directly influences the financial situation of any healthcare environment.
Step 5: Claim Tracking
Managing the healthcare income cycle depends on keeping track of claims. It guarantees that the system can readily handle claims.
After they have been submitted, every claim must be closely monitored. This aids in the identification of any issues or delays in payment processing or rejection causes.
This process can run far faster if one uses contemporary software tools. These instruments give medical professionals real-time data and allow them to monitor several claims concurrently.
Regularly staying in touch with the insurance company could also be vital. As much as feasible, this proactive approach reduces missed income and maintains cash flow consistent.
Tracking also enables one to identify patterns in refused claims. Understanding these trends helps healthcare companies to promptly address issues at their core, therefore improving future outputs and facilitating more effective medical billing procedures generally.
Step 6: Payment Posting
Managing the income cycle in healthcare depends on payment posting in great part. This is the stage in which you record client and insurance company payments. There is a lot at stake here; any errors could lead to issues down the road.
They should be matched to the initial claims sent in after reimbursements are made. This guarantees that every dollar corresponds with both the expected and the paid-for amounts.
Making timely payments helps to maintain consistent cash flow and facilitates the identification of payments either denied or non-made. Errors in filing might compromise the entire medical billing process, therefore affecting collections and delaying their processing.
This phase also facilitates financial reporting and future income change projection for a practice. If providers maintain good records, they will be more aware of their financial situation and make wise judgments moving ahead.
Step 7: Denial Management
Dealing with denials is important in controlling the healthcare income flow. Reversals of claims might cause cash flow to be slowed down and strain the billing staff unnecessarily.
Finding the reason for a rejection of a claim is quite vital. Common causes include coding errors, inadequate record-keeping, or incorrect patient information. Identifying these issues early on will enable speedy correction of them.
Once you understand the nature of the issue, it is time to act. This could mean adjusting the figures or phoning the insurance company to request further information. Frequent clear interaction with payers can help expedite the resolution of problems.
Monitoring denial patterns will also enable you to understand why issues persist. Examining this data helps healthcare companies make adjustments that stop future rejections and quicken their medical billing processes.
Spending time on denial management will result in improved relationships with insurance companies and more income flowing in.
Step 8: Patient Statements and Collections
Managing the revenue cycle depends much on the statements made by patients. Having them facilitates patient and healthcare professional discussion of overdue invoices.
These should be straightforward, direct lists of the offered services and the due values. A clear breakdown of patients’ invoices helps them to better grasp them, hence lowering uncertainty and frustration.
Respect should guide collection efforts. Many consumers could be struggling with money. Providing multiple payment options helps to establish confidence and maintain the money flowing in.
Sending quick notes via email or text message can also help payments be completed faster without being bothersome. By demonstrating that your office values their experience and recognizes how much it costs, an effective collections plan not only addresses cash flow but also makes patients happier.
Healthcare professionals can increase their relationships with patients as well as their revenues by approaching this carefully.
Step 9: Accounts Receivable Follow-Up
Account follow-up Managing the healthcare income cycle depends much on receivables. It guarantees precise and speedy handling of still-owing payments.
At this point, you should monitor claims that haven’t been paid and contact patients or insurers as necessary. Clear communication among people helps to solve problems faster, thereby enabling companies to maintain their cash flow flow.
Healthcare professionals ought to develop a thorough approach for these follow-ups. One approach to accomplish this is to schedule frequent checks on past-due accounts, send letters, or perhaps phone people as needed.
Moreover, using technology might enable this procedure to proceed faster. Automatic monitoring and reminder systems enable staff members more time to care for patients rather than complete documentation and assist in maintaining everything in order.
By demonstrating that you value patients’ financial situation, a proactive approach not only boosts the quantity of payments received but also strengthens the bonds with them.
10: Reporting and Analysis
In the management of healthcare revenue cycles, research and reporting come last stages. Here is where all the data from the earlier steps aggregates to show you the financial situation of your practice. Regularly examining key performance indicators (KPIs) will help you to identify patterns, determine the degree of efficiency of your company, and identify areas for development.
Advanced analytics tools will enable you to view this information. You can consider days until you get paid, the percentage of denied claims, or the patient typical pay. Understanding these elements will help you make wise decisions that will enhance your revenue cycle systems.
Keeping a careful eye on reports helps practices to adjust fast as needed. Reacting fast is vital in the evolving healthcare scene of today. This is true whether your goal is to enhance your collecting techniques following a denials increase or determine the ideal staffing levels depending on volume.
Your medical billing cycle will be more effective and you will generate more money if you pay great attention to every one of the 15 steps above and monitor things by providing comprehensive reports. Changing based on these types of studies not only increases income but also improves the patient experience by simplifying their path through your healthcare system.